
“An 18-year-old England women’s football player tears her ACL 12 weeks prior to the Olympic Games. She is a key player and has been through 4 years of training in preparation and wants to compete. It is an isolated complete ACL tear with no other knee structures damaged. She decides to rehabilitate conservatively rather than having surgery in order to prepare and not miss the games.”
Table of Contents:
- Introduction
- Biomechanics of Football – Predisposing ACL Risk Factors in Women
- Predisposing ACL Risk Factors in Women
- Intrinsic Factors
- Extrinsic Factors
- Goals for Rehabilitation
- Assessment
- Early: Acute Phase of Rehabilitation:
- Middle: Neuromuscular Phase
- Late: Return to Sport Phase
- Return to Sport Assessment
Introduction:
The Olympic Games are a Pinnacle in athletic sporting achievement. In this Essay, we will highlight biomechanics that need to be achieved and avert risk to the Athlete. Predisposing risk factors of the injury and how they will be addressed. Goals of rehabilitation during the 12-week rehabilitation course in the different stages. Strategies and interventions utilised. And a criteria-based evaluation, on when it is appropriate to proceed to the next stage of rehabilitation, return to training, and then to the sport, and competitive play.
Biomechanics of Football – Predisposing ACL Risk Factors in Women
Football consists of a wide range of Skills, that can invariably put the ACL at risk. First it is apt to define the common injury mechanism of the ACL. Direct Contact is seen in 30% of cases. (1) Non-Contact is characterised by 70% of cases (1) in all ACL injuries, and this is predominantly the group associated with football ACL injury. The group that rehabilitation and intervention have the most effect in preventing a re-injury is indeed the non-contact group as neuromuscular control, strength and conditioning play a significant role in prevention of such injuries. (2) Female athletes have a four to six times larger incidence in ACL injury in sports that require cutting and jumping. (3) In women football players it was found to be correlated with more joint laxity and hyperextension in the joints. (4) Joint Hyperextension was found to increase incidence of ACL Injury. (5) Indeed the mechanism for ACL injury, usually involves a “cut and plant” movement, with the leg firmly planted into ground with a vulgus force. Deceleration, and changes in direction are all mechanisms of injury, and prevalent in the biomechanics of football. (6) Walden et al. show that the three most prevalent mechanisms in non-contact ACL injury, involve, “pressing”, “re-gaining balance after kicking” and “landing after a header”. (7) All these situations, often involve unexpected perturbations of balance and sudden landing or unexpected change of direction with the knee hyperextension, or slightly bent in a vulgus rotational force position. (7)
Predisposing ACL Risk Factors in Women
Intrinsic Factors
Stability of the knee is influenced by structural integrity, together with mechanical alignment in movement. Certain intrinsic factors are inherent and non-modifiable. Women have a different pelvic width as well as tibiofemoral angle, to men. (8) A larger Q-Angle in women (9) (Figure- 1) combined with the femoral notch width are considered as significant anatomical factors that predispose women to higher incidence of ACL injury. (10) In theory, a greater Q-Angle predisposes an individual to greater lateral pull of the quadriceps-femoris muscle to the patella causing knee tension medially. Highlighting importance of Quad and hamstring strength.(11)
Figure-1: Static Q Angle
(10)
Hormonal influence in women is also gaining increasing support in the literature for ACL injury as a risk factor with greatest risk of injury identified 1 or 2 days after onset of menses. This information can be used to be more careful with the athlete during that time. (12)
Relative deficits in neuromuscular control, Strength of muscle (13), postural alignment and control (14) as well as landing characteristics (15) also show increased risk in women compared to men. However, they are also regarded as predominantly modifiable. (16) Efficient strength and conditioning programs, and athletic specific training showsignificant promise in influencing possible deficits. (17) Knee stiffness is also considered a significant conjunct to knee stability as well as injury prevention. Mechanoreceptors can modulate joint ligamentous and muscle laxity stiffness. (18)
Extrinsic Risk Factors
There are several factors of extrinsic risk, many are non-modifiable, however important to consider, to safely return the athlete to sport. Things like surface and shoe type, pitch type. Working from hard steady ground with athletic trainers, to grass pitch, and the use of football cleats. Lambson at al. (1996) show that football cleats increase traction substantially, and this has a corelative effect with increased incidence of ACL injury. (19) Other factors include, the general fitness level of elite Olympic women’s football players. Our patient, must be ready to play in 12 weeks, and as such must maintain a fitness level that would not put her at increased risk of injury, but also be able to maintain and perform at the required cardiovascular strength and speed, of the game she is being prepared for, and therefore must maintain her fitness pre-injury and build on it. (20) (21) These factors must all be considered, into the return to sport training phase.
Goals for Rehabilitation
Focus should be targeted towards modifiable intervention, which will focus primarily on prevention of non-contact (loosely defined as non-direct outside force to knee structure) as well as catered specifically for the demands and level of the sport and level of play (elite women’s football – Olympics). A Physiological and Psychological assessment should be conducted for return to play, and to manage expectations and motivation throughout the process, as only a small percentage of players will be able to return to pivoting and cutting sports without knee-reconstruction. (22)
Assessment
Conservative ACL Rehab treatment can be considered since there are no other concomitant injury. In order for non-operative treatment of ACL rehabilitation to return to cutting and pivoting sports, it is necessary to identify “Potential coppers”. This is done through a number of screening tests. (23) As seen in Table-1
Table 1: Screening tests of “Coppers vs Non-Coppers” suitable for ACL non-operative
| Testing | Potential Coppers |
| Knee Screening; Physical Exam; Subjective/Objective | No other concomitant injury |
| Hop testing. (One legged distance, triple hop, cross over hp and 6m timed hop test). | Minimum of 80% limb symmetry |
| Knee giving way report | |
| Self-reported global knee function rating. | >60 |
| Knee Outcome survey/Activity of Daily Living scale | >80% |
(23)
The screening tests are vital if the patient wants to return to Cutting/pivoting sport. If they cannot meet it is more likely they will have to reduce physical activity and be classified as a ‘Non-copper’. (24) Our patient has been identified as a Copper.
Figure-2: Hop-Testing
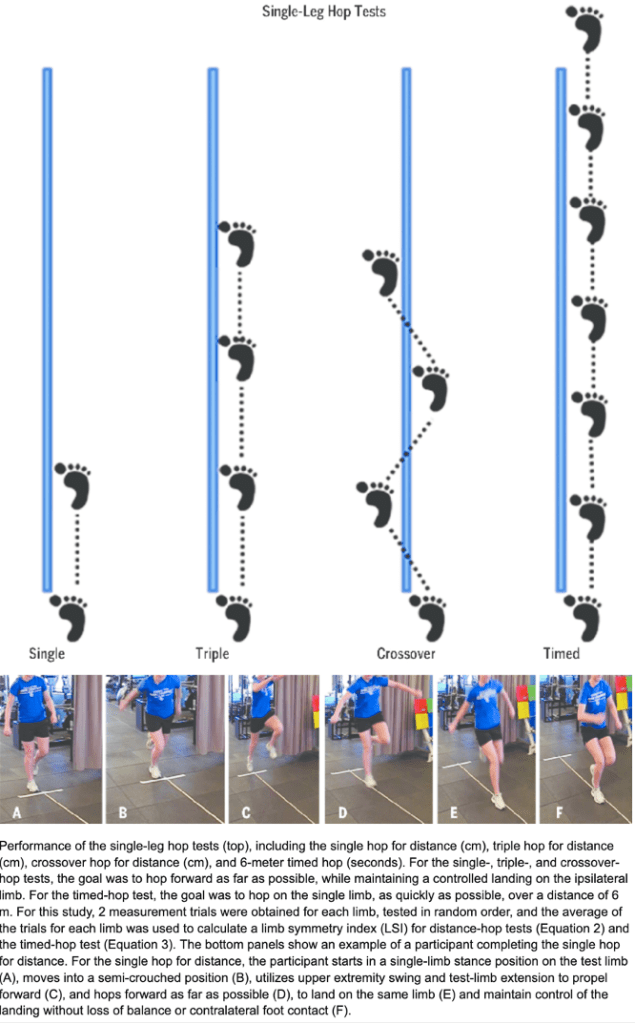
(25)
Early: Acute Phase of Rehabilitation:
Homeostasis; ROM Muscle Activation: Focus on restoration of joint homeostasis and Active Range of motion (ROM). Hemarthrosis must be reduced. Cryotherapy and compression help in an aggressive approach to manage acute effusion. (26)
Goals:
Activation: Improve integrity of motion and muscle activation. Utilisation of wall slides as well as stationary bike. Can start also with quadricep isometric contraction. (10) Facilitation of Patellofemoral glide through manual therapy and activation of Quadriceps, and NMES (27) in medio-cephalic direction is desirable (28) (29).
Strength: A focus on quadriceps should utilise open chain exercise (OKC) and closed kinetic chain (CKC) should be utilised together as tolerated as OKC targets isolated quadriceps whilst CKC has more dynamic application. OKC limited to 30-100
flexion to reduce “anterior shearing” in knee. (30)
Strength training in acute phase should also address any identified weakness in hamstring, hip and core. (31) Any deficits in trunk control are a significant risk to re-injury and should be addressed. (32)
Middle: Neuromuscular Phase
Progression Indicators: Effusion controlled, Achieved full ROM, Base lower extremity strength allowing for participation in more dynamic weight bearing exercise. (32)
Goals: Continued focus on lower extremity strength, with addition of neuromuscular training, balance, proprioception, stability, continue strength building, and move into power as well as maintain and build Cardio-vascular requirements, for football. (32) Elite athletes must maintain, and progress fitness and strength in non-injured sites.
Perturbation Exercise: Literature shows significant efficacy of putting patients on surfaces challenging their balance state, and unexpected perturbations utilised to challenge their ability to maintain balance. (33)
Figure 3: Perturbation Training

(34)
Late: Return to Sport Phase
Progression Indicators: No Episodes of “giving way” during neuromuscular phase. Hamstring and Quadricep strength must have advanced and demonstrated through isometric testing as 90% of contra-lateral limb. (32)
Goals: Return to play to cutting and pivoting must be geared to sport specific integration of sport. This must be done systematically and gradually. There is evidence that a brace, can help in accommodating this transition and accommodating patient stability reducing anterior tibial translation and proprioceptive feedback. (35)
Figure-4: Cutting and Pivoting Drill for 6 weeks Resulted in Meaningful results in youth Soccer Players. (35)
(36)
Stages: Continue with straight line running at non-maximal speed, that is slowly progressed to changes in direction and running in various planes of movement eventually progressing to full speed changes of direction (37), and then integrated to sport specific movements, ball control, kicking the ball. Finally progress to injury vulnerable states of loading, to facilitate a safe return and avoid re-injury. (38) Cardiovascular and strength training and requirements of activity must be simultaneously maintained, as the athlete must return to elite level sport, and is expected to meet the cardiorespiratory and fitness requirements. (32)
Return to Sport Assessment
Return to sport testing and assessment should be conducted through an objective analysis of lower limb strength, functional kinematics as well as ability to integrate to specific demands of the sport. Physiological (39) and psychological readiness also play a significant role. (32) Isokinetic strength of Quadriceps and hamstrings, as well as hop tests described in initial assessment should have >90% co-symmetry. (40) (41).
Tuck Jump and single leg squat assessments can be used to test asymmetries. (42)
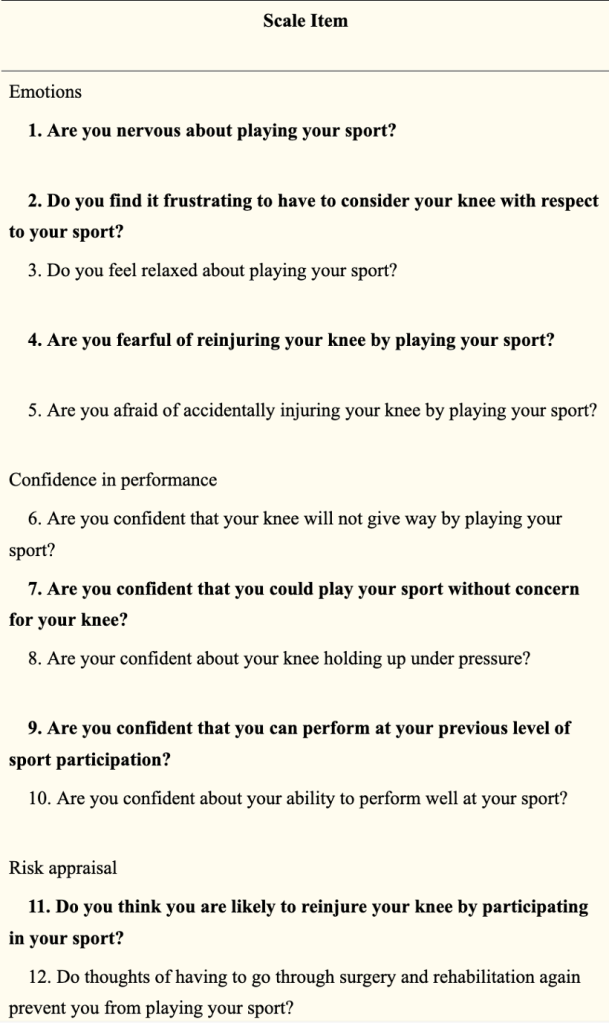
For the Psychological component we can use the “12-Item ACL-Return to Sport (ACL-RSI) scale”. (39)
Sport Specific readiness assessed through systematic increases of load and subjective monitoring, of sport specific functions movement, and fitness levels.
Figure-5: (ACL-RSI) scale
Conclusion
The goal is to return the player safely to her sport, by considering all the risk factors, both intrinsic and extrinsic and working towards strength, neuromuscular control, inherent dynamics of football which is a cutting and pivoting sport. The athlete must be able to take on all the demands the sport can put them under, with increased loads and eventual stressing of knee towards loads and positions that could be considered injury vulnerable states. The physiotherapist must be happy with the athlete’s progression at every stage before giving the clear and go ahead to progress, objectively as well as subjectively, and utilize a diagnostic approach. (43) The athlete can-not progress without reaching each goal set for him, even if time is constrained. One vital aspect not often considered is the athletes psychological state, after the rehabilitation is completed. (32) The athlete must also have confidence in the work put in, therefore the athletes psychological state in itself should be the final barrier to overcome once the therapist is happy with achievement of his physiological sport-specific objectives.
References:
1. McNair PJ, Marshall RN, Matheson JA. Important features associated with acute anterior cruciate ligament injury. N Z Med J. 1990;103(901):537-9.
2. Dhillon H, Dhillon S, Dhillon MS. Current Concepts in Sports Injury Rehabilitation. Indian J Orthop. 2017;51(5):529-36.
3. Hewett TE, Myer GD, Ford KR. Anterior Cruciate Ligament Injuries in Female Athletes. The American Journal of Sports Medicine. 2006;34(2):299-311.
4. Wojtys EM, Huston LJ, Lindenfeld TN, Hewett TE, Greenfield MLV. Association between the menstrual cycle and anterior cruciate ligament injuries in female athletes. The American journal of sports medicine. 1998;26(5):614-9.
5. Hewett TE, Myer GD, Ford KR, Paterno MV, Quatman CE. Mechanisms, prediction, and prevention of ACL injuries: Cut risk with three sharpened and validated tools. Journal of Orthopaedic Research. 2016;34(11):1843-55.
6. Pfeifer CE, Beattie PF, Sacko RS, Hand A. RISK FACTORS ASSOCIATED WITH NON-CONTACT ANTERIOR CRUCIATE LIGAMENT INJURY: A SYSTEMATIC REVIEW. Int J Sports Phys Ther. 2018;13(4):575-87.
7. Waldén M, Krosshaug T, Bjørneboe J, Andersen TE, Faul O, Hägglund M. Three distinct mechanisms predominate in non-contact anterior cruciate ligament injuries in male professional football players: a systematic video analysis of 39 cases. British Journal of Sports Medicine. 2015;49(22):1452-60.
8. HUNGERFORD DS, BARRY M. Biomechanics of the Patellofemoral Joint. Clinical Orthopaedics and Related Research®. 1979(144):9-15.
9. Hahn T, Foldspang A. The Q angle and sport. Scand J Med Sci Sports. 1997;7(1):43-8.
10. Huston LJ, Greenfield MLVH, Wojtys EM. Anterior Cruciate Ligament Injuries in the Female Athlete: Potential Risk Factors. Clinical Orthopaedics and Related Research®. 2000;372:50-63.
11. SHAMBAUGH JP, KLEIN A, HERBERT JH. Structural measures as predictors of injury in basketball players. Medicine & Science in Sports & Exercise. 1991;23(5):522-7.
12. Slauterbeck JR, Fuzie SF, Smith MP, Clark RJ, Xu K, Starch DW, et al. The Menstrual Cycle, Sex Hormones, and Anterior Cruciate Ligament Injury. J Athl Train. 2002;37(3):275-8.
13. Griffin JW, Tooms RE, vander Zwaag R, Bertorini TE, O’Toole ML. Eccentric muscle performance of elbow and knee muscle groups in untrained men and women. Med Sci Sports Exerc. 1993;25(8):936-44.
14. Huston LJ, Wojtys EM. Neuromuscular performance characteristics in elite female athletes. Am J Sports Med. 1996;24(4):427-36.
15. Colby S, Francisco A, Yu B, Kirkendall D, Finch M, Garrett W, Jr. Electromyographic and kinematic analysis of cutting maneuvers. Implications for anterior cruciate ligament injury. Am J Sports Med. 2000;28(2):234-40.
16. Caraffa A, Cerulli G, Projetti M, Aisa G, Rizzo A. Prevention of anterior cruciate ligament injuries in soccer. A prospective controlled study of proprioceptive training. Knee Surg Sports Traumatol Arthrosc. 1996;4(1):19-21.
17. Hewett TE, Stroupe AL, Nance TA, Noyes FR. Plyometric training in female athletes. Decreased impact forces and increased hamstring torques. Am J Sports Med. 1996;24(6):765-73.
18. Sojka P, Sjolander P, Johansson H, Djupsjobacka M. Influence from stretch-sensitive receptors in the collateral ligaments of the knee joint on the gamma-muscle-spindle systems of flexor and extensor muscles. Neurosci Res. 1991;11(1):55-62.
19. Lambson RB, Barnhill BS, Higgins RW. Football cleat design and its effect on anterior cruciate ligament injuries: a three-year prospective study. The American journal of sports medicine. 1996;24(2):155-9.
20. Njororai Simiyu W. Physical demands of soccer: Lessons from team USA and Ghana matches in the 2010 FIFA WORLD CUP. Journal of Physical Education and Sport. 2012;12:407-12.
21. Ingebrigtsen J, Dillern T, Shalfawi SA. Aerobic Capacities and Anthropometric Characteristics of Elite Female Soccer Players. The Journal of Strength & Conditioning Research. 2011;25(12):3352-7.
22. Fabricant PD, Lakomkin N, Cruz AI, Spitzer E, Marx RG. ACL reconstruction in youth athletes results in an improved rate of return to athletic activity when compared with non-operative treatment: a systematic review of the literature. 2016;1(2):62-9.
23. Soltani N, Rahimi A, Naimi S-S, Khademi K, Saeedi H. Studying the Balance of the Coper and Non-Coper ACL-Deficient Knee Subjects. Asian J Sports Med. 2014;5(2):91-8.
24. Hurd WJ, Axe MJ, Snyder-Mackler L. A 10-year prospective trial of a patient management algorithm and screening examination for highly active individuals with anterior cruciate ligament injury: Part 2, determinants of dynamic knee stability. The American journal of sports medicine. 2008;36(1):48-56.
25. Schmitt L, Paterno M, Hewett T. The Impact of Quadriceps Femoris Strength Asymmetry on Functional Performance at Return to Sport Following Anterior Cruciate Ligament Reconstruction. The Journal of orthopaedic and sports physical therapy. 2012;42:750-9.
26. Hurd W, Axe M, Snyder-Mackler L. Management of the athlete with acute anterior cruciate ligament deficiency. Sports Health. 2009;1(1):39-46.
27. Snyder-Mackler L, Ladin Z, Schepsis AA, Young J. Electrical stimulation of the thigh muscles after reconstruction of the anterior cruciate ligament. Effects of electrically elicited contraction of the quadriceps femoris and hamstring muscles on gait and on strength of the thigh muscles. The Journal of bone and joint surgery American volume. 1991;73(7):1025-36.
28. Suter E, McMorland G, Herzog W, Bray R. Conservative lower back treatment reduces inhibition in knee-extensor muscles: a randomized controlled trial. Journal of Manipulative and Physiological Therapeutics. 2000;23(2):76-80.
29. Bousquet B, O’Brien L, Singleton S, Beggs M. POST-OPERATIVE CRITERION BASED REHABILITATION OF ACL REPAIRS: A CLINICAL COMMENTARY. Int J Sports Phys Ther. 2018;13.
30. Beynnon BD, Fleming BC, Johnson RJ, Nichols CE, Renström PA, Pope MH. Anterior cruciate ligament strain behavior during rehabilitation exercises in vivo. The American Journal of Sports Medicine. 1995;23(1):24-34.
31. Hewett TE, Torg JS, Boden BP. Video analysis of trunk and knee motion during non-contact anterior cruciate ligament injury in female athletes: lateral trunk and knee abduction motion are combined components of the injury mechanism. British journal of sports medicine. 2009;43(6):417-22.
32. Paterno MV. Non-operative Care of the Patient with an ACL-Deficient Knee. Curr Rev Musculoskelet Med. 2017;10(3):322-7.
33. Chmielewski TL, Rudolph KS, Snyder-Mackler L. Development of dynamic knee stability after acute ACL injury. Journal of Electromyography and Kinesiology. 2002;12(4):267-74.
34. Hurd WJ, Chmielewski TL, Snyder-Mackler L. Perturbation-enhanced neuromuscular training alters muscle activity in female athletes. Knee Surgery, Sports Traumatology, Arthroscopy. 2006;14(1):60-9.
35. Beynnon BD, Fleming BC, Churchill DL, Brown D. The effect of anterior cruciate ligament deficiency and functional bracing on translation of the tibia relative to the femur during nonweightbearing and weightbearing. The American journal of sports medicine. 2003;31(1):99-105.
36. Dos’Santos T, McBurnie A, Comfort P, Jones PA. The Effects of Six-Weeks Change of Direction Speed and Technique Modification Training on Cutting Performance and Movement Quality in Male Youth Soccer Players. Sports. 2019;7(9):205.
37. Fitzgerald GK, Axe MJ, Snyder-Mackler L. Proposed practice guidelines for nonoperative anterior cruciate ligament rehabilitation of physically active individuals. Journal of Orthopaedic & Sports Physical Therapy. 2000;30(4):194-203.
38. Blanch P, Gabbett TJ. Has the athlete trained enough to return to play safely? The acute: chronic workload ratio permits clinicians to quantify a player’s risk of subsequent injury. Br J Sports Med. 2016;50(8):471-5.
39. Webster KE, Feller JA, Lambros C. Development and preliminary validation of a scale to measure the psychological impact of returning to sport following anterior cruciate ligament reconstruction surgery. Physical therapy in sport. 2008;9(1):9-15.
40. Ithurburn M, Paterno M, Ford K, Hewett T, Schmitt L. QUADRICEPS FEMORIS STRENGTH ASYMMETRY DIFFERENTIATES SINGLE-LEG DROP-LANDING MECHANICS AT RETURN TO SPORT IN YOUNG ATHLETES AFTER ANTERIOR CRUCIATE LIGAMENT RECONSTRUCTION: SPL34. journal of Orthopaedic & Sports Physical. 2015;45(1).
41. Nagai T, Schilaty ND, Laskowski ER, Hewett TE. Hop tests can result in higher limb symmetry index values than isokinetic strength and leg press tests in patients following ACL reconstruction. Knee Surgery, Sports Traumatology, Arthroscopy. 2020;28(3):816-22.
42. Myer GD, Ford KR, Hewett TE. Tuck jump assessment for reducing anterior cruciate ligament injury risk. Athletic therapy today: the journal for sports health care professionals. 2008;13(5):39.
43. Weiler R, Monte-Colombo M, Mitchell A, Haddad F. Non-operative management of a complete anterior cruciate ligament injury in an English Premier League football player with return to play in less than 8 weeks: applying common sense in the absence of evidence. BMJ Case Reports. 2015;2015:bcr2014208012.
Exercise Program:
Acute Phase:
Rehabilitation must be outcome based. And cannot proceed without goals and progression indicators being met.
The following is a retrospective Hypothetical Progression Scenario.
Week 1-4
Relative rest, elevation, cryotherapy to Reduce swelling and inflammation.
Ice 3-5 times a day, for 30 minutes.
Patella mobilisations and glides.
Restore Voluntary muscle Activation. Activate VMO medially and upwards. 5x10s holds
Activation: Improve integrity of motion and muscle activation. Utilisation of wall slides as well as stationary bike. Can start also with quadricep isometric contraction. (10) Facilitation of Patellofemoral glide through manual therapy and activation of Quadriceps, and NMES (27) in medio-cephalic direction is desirable (28) (29).
Strength: A focus on quadriceps should utilise open chain exercise (OKC) and closed kinetic chain (CKC) should be utilised together as tolerated as OKC targets isolated quadriceps whilst CKC has more dynamic application. OKC limited to 30-100
flexion to reduce “anterior shearing” in knee. (30)
Exercises Acute Phase:
| | Goals | Monday-Sunday Exercise: | Exercise: | Repetitions 5 Times per day |
| Reduce Swelling | Ice | 30 min 5 times per day | ||
| Reduce Swelling | Elevation Whenever possible, Keep above Heart level | Whenever resting | ||
| Knee Extension | Active-Assisted Extension, Using opposite leg to straighten quadriceps 90 – 0 degrees Avoid hyperextension | 5 times, 30 second hold end range. | ||
| Increase Range of Motion | Wall slides, PROM Lie on back injured leg on wall | Slowly slide leg down Hold max flexed position 30 seconds – Repeat 5 times | ||
| Quadricep Activation | Activation of quad (VMO) Gain Extension ROM Upwards and mediaal activation and hold Isometric Hold | !0-15 Reps !0 Second hold 3 Sets | ||
| Gain ROM – Flexion | Leg Slides on bed. | Pull heel towards buttocks |
Week 2:
| Week 2 | Goals | Monday-Sunday Exercise | exercise | Repetitions/Once Daily Unless otherwise Indicated |
| Continue Week 1 Exercises | Week 1 Exercises | Week 1 Exercises | Week 1 exercises | |
| 100 Degree Flexion Achieved ROM Increase Strength Minimal resistance | Cycling | 20 Mins Twice daily | ||
| Straigh leg raise Strength quad | SLR – Side to Side – down | 3 Sets 15 Repetions | ||
| Glute Strength Core Strength | Hip Extension/Bridge | 3 sets 15 Repetions | ||
| Hip Abd/Add/ | Hip Abd/Add | 3 sets 15 Repetions | ||
| Quad Strength Glute strength Partial range | Body Weigh Squats | 2-3 Sets 10-20 Repetitions | ||
| Quad Strength Hamstring eccentiric | Standing TKE with Theraband/cable | 3 Sets 15 Repetions | ||
| Hamstring Stength | Standing or prone hamstring curls | 3 Sets of 15 Repetitions | ||
| Gastroc Strengthening | Heel raises | 3 Sets of 15 Repetitions | ||
| Start low impact, cardio, sport Specific. | Anti-gravity Run (70% body weight, progressed to 80 then 90) | 30 mins Once a day 5x per week Start at walk work to jog |
Wekk 3-4
| Week 3-4 | Goals: Progression | Monday-Sunday Exercise | exercise | Perform Strengthening Exerices 3-5 Times a week. |
| 100 Degree Flexion Achieved ROM Increase Strength Minimal resistance | Cycling | 20 Mins Once a day 5x per week | ||
| Improme ROM/Flexibility | “Continue ROM/Flexibility Exercises “ | Week 1 Exercises | Work on ROM as per week 1 | |
| Continue Open Chain/Progress with increased weight. | Hip/Knee Exercises | Week 2 Exercises | Week 2 exercises | |
| Quad & Hamstring strength Exercise Progression | Hamstring Curl Machine Quadricep Machine | 3 Sets 12 rep 70%!RM – 3x week | ||
| Leg Press | Leg Press (Progress double-Single leg) | 3 sets 12 reps 3x per week 70% !RM | ||
| Quad glute Strengthening/ Stability | Hamstring strength Exercise Progression (foreward and lateral) | 3 sets 15 reps 3x per week | ||
| Glutes Quads, Stability, Core | Squat 90 degrees | 3 Sets 12 reps 80%1RM3x per week | ||
| Core stability | Plank/Side-plank | 2 Sets 30 seconds 5x per week | ||
| Gluts, core stability control hip extensor. | Single Limb Bridge | 2 Sets 15 seconds 5x per week | ||
| Begin Proprioception Training Progress to eyes closed | Bosu half Ball | 30-60 seconds 5 times per week | ||
| Start low impact, cardio, sport Specific. | Anti-gravity Run (70% body weight, progressed to 80 then 90) | 20 mins Once a day 5x per week Start at low Impact |
Middle: Neuromuscular Phase
Progression Indicators: Effusion controlled, Achieved full ROM, Base lower extremity strength allowing for participation in more dynamic weight bearing exercise. (32)
Goals: Continued focus on lower extremity strength, with addition of neuromuscular training, balance, proprioception, stability, continue strength building, and move into power as well as maintain and build Cardio-vascular requirements, for football. (32) Elite athletes must maintain, and progress fitness and strength in non-injured sites.
Perturbation Exercise: Literature shows significant efficacy of putting patients on surfaces challenging their balance state, and unexpected perturbations utilised to challenge their ability to maintain balance. (33)
| Monday | Lower body strength & cardio |
| Tuseday | Lower body (week 4-6)/Plyometrics (week 6-8) & upper body strength |
| Wednesday | Low load recovery (core stability-Perturbation) & cardio |
| Thursday | Same as Monday |
| Friday | Same as Tuseday |
| Saturday | Same as Wednesday |
| Sunday | Off |
Lower Body Strength:
| Week 4-8 | Middle: Neuromuscular Phase | Exercise – Lower Body Strength | exercise | Neuromuscular & Strength |
| 100 Degree Flexion Achieved ROM Increase Strength Minimal resistance | Cycling | 20 Mins | ||
| Glutes Quads, Stability, Core | Squat 90 degrees | 3 Sets 12 reps 80%1RM Progression: Build power Drop reps to 6; Increase load | ||
| Quad glute Strengthening/ Stability | strength Exercise Progression (foreward and lateral) | 3 sets 15 reps Progression: Include Weights 3 sets 6 Reps | ||
| Hamstring Isolation | Nordics | 2 sets 5 Reps Progress Reps Sets over time. | ||
| Quad Isolation StrengthHamstring Isolation Strength | Quadricep Machine Hamstring Machine | 3 sets 10-15 Reps 80% 1 RM | ||
| Build Quad, and Glute strength Slow eccentric down | Leg Press (Progress double-Single leg) | 3 sets 12 reps 3x per week 80% !RM Progression slowly to Power 3 sets 6 reps | ||
| Quad Strength/ Neuromuscular control/ decceleration | Weighted Walking Lunge | 3 sets 12 reps Progresison, lower reps, increase weight | ||
| Adductor strengthening | Coppenhagens | 3-5 sets; 5-20 reps Progression | ||
| Gastroc Strengthening | Heel raises | 3 Sets of 15 Repetitions Progression Power 3 sets 6 rep Increase Load | ||
| Warm down | Warm Down – slow cycle Passive stretch/Foam roller | 10 mins |
Cardio:
| Week 4-8 | Middle: Neuromuscular Phase | Exercise – Cardiorespiratory | exercise | Sets Reps |
| Warm Up | Jog – 1500m Dynamic Stretching through full ROM | 1- 1500m (Slow pace) High knees Christie Walks Deep Squad stretches Side to side Backwards run Touch ground slow run Kick ups | ||
| Interval Jogging/Sprints | 200m Jog, Followed by 200m Sprint | 60% Max Progress intensity over time 6-8 reps | ||
| Accelerate/Deccelerate Straight line running. | 20m Runs Cone to cone Progression Add 10m interval Cut sets in half, increase speed. | Start 60% of Sprint Progress in intensity 20 sets x 2 | ||
| Endurance | 400m Sprint | 60% max Progress to 100% 3-4 reps | ||
| Neuromuscular control | Cone Runs | 15 reps/3sets/ 10m | ||
| Warm Down | 1500m Light jog Light Static Stretching recovery | 1 Run Hamstring/Quad/add stretch Stretch for recovery as needed. |
Lower Impact Introduction for Plyometrics – Neuromuscular
| Week 6-8 | Middle: Neuromuscular Phase | Exercise – Plyometrics | exercise | Sets Reps |
| Warm Up | Jog – 1500m Dynamic Stretching through full ROM | 1- 1500m (Slow pace) High knees Christie Walks Deep Squad stretches Side to side Backwards run Touch ground slow run Kick ups | ||
| Velocity and eccentric neuromusclular control/ Power | Vertical Box Step up | 10 reps/3 sets | ||
| Velocity and eccentric neuromuscular control | Single leg Side Box over Jump | 10 reps/2sets | ||
| Neuromuscular technique landing, Safe, deceleration | Double Jump ForewordFocus on Neuromuscular control and technique | 5 Jumps/3 sets 60% max | ||
| Increase explosive force with low impact Eccentric control down | Stair climbs | 10 repetitions (±20 stairs) | ||
| Neuromuscular Control and stability | Side to side Jump and hold | 15 reps/3 sets | ||
| Warm Down | 1500m Light jog Light static stretch Recovery | Hamstring/Quad/add stretch Stretch for recovery as needed. |
Upper Body
| Week 4-8 | Goals: Progression | Upper Body | exercise | Sets Reps |
| Warm Up | Upper body Ergometer | 1- 1500m (Slow pace) Arm rolls Spider man walks knee to elbow | ||
| Pectoral Strength. Slow down, eccentric Control. | Bench Press | 2 Sets 12-15 reps Rest 60 Seconds 80% !RM | ||
| Build Stability in upper Limb & Core | Side Plank | 2 Sets 10-15/side Rest 60 Seconds | ||
| Ant- Deltiod & Stability | Front Arm Raises | Sets: 2 Reps 12-15 80%1RM Rest 60 Seconds | ||
| Stability, and Upper body velocity/functional | Medicine ball throw | Sets: 2 Reps 8-12 Rest 60 Seconds | ||
| Stability control Pectoral strength Anterior Deltoid Triceps | Incline DB Press | Sets 2 Reps: 8-12 80% 1RM | ||
| Lattismus Dorsi Rhomboids, Scapular Stabilizer, Spinal Erectors | Rows | Sets: 2 8-12 Reps 80% 1RM | ||
| Middle fibres of trapezius Stabilizers | Shrugs | Sets: 2 Reps 12-15 80%1RM Rest 60 Seconds | ||
| Deltoid, Trapezius, Serratus and terior Core stabilisation | Military Press | Sets: 2 Reps 12-15 80%1RM Rest 60 Seconds | ||
| Warm Down | 1500m Light jog Light static stretch Recovery | Hamstring/Quad/add stretch Stretch for recovery as needed. |
Core Stability – Perturbation
| Week 4-8 | Goals: Progression | Stability – Perturbation | exercise | Sets/Reps |
| Increase HR | Warm- up – Cycling | 15 mins | ||
| Functional dynamic activation | 3- step Hold stabilise Backwards and foreward High Knee skips Back Pedals Lateral Lunge walks Single leg alternating holds Single leg lift | Functional Movements, 20m Each | ||
| Achieve balance, stability Advance with ball throw | Single leg Bosu exercise Balance. | 30 second x 10 reps | ||
| Rectus abdominus; Stability Functional, Core. | Sit ups with medicine ball throw | Reps 15 Sets 3. | ||
| Core stability, Hip flexors, Eccentric load contro With Press up.l | TRX Forward facing full body Flexion. | Reps 15 Sets 3 | ||
| Functional/dynamic Stability | Pertubation: Box up with Directional offbalance. | Reps 15 Sets 2 | ||
| Stability balance SL Pertubation | Single leg hold squat. | Hold 30 seconds – 5 times, Each leg | ||
| Stability Control | Side Plank | 30 second x 3 reps | ||
| Stability Control | Front Plank | 30 seconds x 3 reps | ||
| Stability, and movement, all 4 limbs | All 4’s Hold follow ball | 30 seconds x 3 reps | ||
| Neuromusclular control, and fulll body core, and stability | Bosu ball front facing Crunch | 15 Reps 3 sets | ||
| Warm down | Warm Down – slow cycle Passive stretch/Foam roller | 10 mins |
Late: Return to Sport Phase Week 8-11
Progression Indicators: No Episodes of “giving way” during neuromuscular phase. Hamstring and Quadricep strength must have advanced and demonstrated through isometric testing as 90% of contra-lateral limb. (32)
Progress to power, when athlete is able to Run/jog on Anti-Gravity treadmill at least 90 percent Gravity; Squat 80% of 80% of 10 RM, Leg at 4cm dif of Y-test. Hamstring Quad ration at 60% on dynamometer. (32)
Goals: Return to play to cutting and pivoting must be geared to sport specific integration of sport. This must be done systematically and gradually. There is evidence that a brace, can help in accommodating this transition and accommodating patient stability reducing anterior tibial translation and proprioceptive feedback. (35)
Stages: Continue with straight line running at non-maximal speed, that is slowly progressed to changes in direction and running in various planes of movement eventually progressing to full speed changes of direction (37), and then integrated to sport specific movements, ball control, kicking the ball. Finally progress to injury vulnerable states of loading, to facilitate a safe return and avoid re-injury. (38) Cardiovascular and strength training and requirements of activity must be simultaneously maintained, as the athlete must return to elite level sport, and is expected to meet the cardiorespiratory and fitness requirements. (32)
| Monday | Lower body Power & Sport Specific Cardio |
| Tuseday | Plyometrics & upper body strength |
| Wednesday | Low load recovery (Sport Specific-Perturbation-Stability) & Sport Specific cardio |
| Thursday | Same as Monday |
| Friday | Same as Tuseday |
| Saturday | Same as Wednesday |
| Sunday | Off |
Lower Body Power
| Week 8-11 | Middle: Neuromuscular Phase | Exercise – Lower Body Power | exercise | Neuromuscular & Strength |
| 100 Degree Flexion Achieved ROM Increase Strength Minimal resistance | Cycling | 20 Mins | ||
| Glutes Quads, Stability, Core | Squat 90 degrees | 3 Sets 4-6 reps 80%1RM Progression: Build power Drop reps to 6; Increase load | ||
| Quad glute Strengthening/ Stability | Lunges with Weight | 3 sets 4-6 reps 90% 1RM | ||
| Hamstring Isolation | Nordics | 2 sets 5 Reps Progress Reps Sets over time. | ||
| Quad Isolation | Quadricep Machine | 3 sets 4-6 Reps 80% 1 RM | ||
| Build Quad, and Glute strength Slow eccentric down | Leg Press (Progress double-Single leg) | 3 sets 4-6 reps 3x per week 90% 1RM | ||
| Quad Strength/ Neuromuscular control/ decceleration | Weighted Walking Lunge | 3 sets 12 reps Progresison, lower reps, increase weight | ||
| Adductor strengthening | Coppenhagens | 3-5 sets; 5-20 reps Progression | ||
| Gastroc Strengthening | Heel raises | 3 Sets of 4-6 Repetitions | ||
| Warm down | Warm Down – slow cycle Passive stretch/Foam roller | 10 mins |
Upper Body:
| Week 4-8 | Goals: Progression | Upper Body | exercise | Sets Reps |
| Warm Up | Upper body Ergometer | | 1- 1500m (Slow pace) Arm rolls Spider man walks knee to elbow | |
| Pectoral Power. Slow down, eccentric Control. | Bench Press | 2 Sets 12-15 reps Rest 60 Seconds 80% !RM | ||
| Build Stability in upper Limb & Core | Side Plank | 2 Sets 10-15/side Rest 60 Seconds | ||
| Ant- Deltoid Power | Front Arm Raises | Sets: 3 Reps 4-6 90%1RM Rest 60 Seconds | ||
| Stability, and Upper body velocity/functional – Power | Medicine ball Slam | | Sets: 4 Reps 4-6 Rest 60 Seconds | |
| Stability control Pectoral strength Anterior Deltoid Triceps | Incline DB Press | Sets 3 Reps: 4-6 90% 1RM | ||
| Lattismus Dorsi Rhomboids, Scapular Stabilizer, Spinal Erectors | Rows | Sets: 3 4-6 Reps 80% 1RM | ||
| Middle fibres of trapezius Stabilizers | Shrugs | Sets: 3 Reps4-6 90%1RM Rest 60 Seconds | ||
| Deltoid, Trapezius, Serratus and terior Core stabilisation | Military Press | | Sets: 3 Reps4-6 90%1RM Rest 60 Seconds | |
| Warm Down | 1500m Light jog Light static stretch Recovery | Hamstring/Quad/add stretch Stretch for recovery. |
Plyometrics
| Week 8-11 | Late: RTP | Exercise – Plyometrics | exercise | Sets Reps |
| Warm Up | Jog – 1500m Dynamic Stretching through full ROM | | 1- 1500m (Slow pace) High knees Christie Walks Deep Squad stretches Side to side Backwards run Touch ground slow run Kick ups | |
| Quick Explosive speed | 1 in 1 Out Ladder | 15 times, Quick | ||
| Absorb landing, and Explosive vertical jump | Depth Box Jump | | 10 reps 3 sets | |
| Increase Velocity/power | Vertical Box Jump land Double leg | 10 reps/3 sets | ||
| Increase Velocity/power | Tuck Jumps | 10 reps/2sets | ||
| Increase Velocity/power landing, Safe, deceleration | Standing Long Jump | 6 Jumps/3 sets 60% max | ||
| Work On Change of direction Technique, and explosive change of direction | Cut and Plant, Cone runs Quick steps | | 20 repetitions | |
| Greater Power progression | Ice Skaters Side to side Jump and hold | 15 reps/3 sets | ||
| Warm Down | 1500m Light jog Light static stretch Recovery | Hamstring/Quad/add stretch Stretch for recovery as needed. |
Sport Specific – Conditioning:
| Week 8-11 | Late: RTP | Exercise – Field Training | exercise | Sets Reps |
| Warm Up | Jog – 1500m Dynamic Stretching through full ROM | 1- 1500m (Slow pace) High knees Christie Walks Deep Squad stretches Side to side Backwards run Touch ground slow run Kick ups | ||
| Interval Speed | 40m Sprint | 80-90% Max Progress intensity over time 15 reps | ||
| Accelerate/Deccelerate Straight line running. | 20m Runs Cone to cone Progression Add 10m interval | Start 90% of Sprint 20 sets | ||
| Reaction/Agility Movement | Reaction Agility Box Jump down: Pass Ball/Header one direction on Cue Run other | 20 reps x 2 – Run 10m Back. | ||
| Build fitness/Speed/Cardio | 200m Sprint | 5 Reps 80% Sprint | ||
| Sport Specific Shooting, passing skills – Off-balance progression with Pertubation | Shooting/Passing With Coaching team; Add Pertubation | N/A | ||
| Focus on Cutting Changing direction Progression add Ball | 4D Cone Runs | 15 resp/3sets/5x5x5 | ||
| Warm Down | 1500m Light jog Light Static Stretching recovery | 1 Run Hamstring/Quad/add stretch Stretch for recovery as needed. |
Sport Specific-Perturbation-Stability
| Week 8-11 | Goals: Progression | Stability – Perturbation+C:C | exercise | Sets/Reps |
| Increase HR | Warm- up – Cycling | 15 mins | ||
| Functional dynamic activation | 3- step Hold stabilise Backwards and foreword High Knee skips Back Pedals Lateral side to side Single leg alternating holds Single leg lift | Functional Movements, 20m Each | ||
| Achieve balance, stability Advance with Verbal Cue for which cone | Single leg Bosu exercise Balance – 1 leg Reach and touch cones | 30 second x 10 reps | ||
| Stability, with unexpected force. | Step Down with Perturbation | Reps 15 Sets 3. | ||
| Progress to One Leg | TRX Forward facing full body Flexion. | Reps 15 Sets 3 | ||
| Functional/dynamic Stability | Tennis football- All fours – Competitive Non-contact game | 1 minute: 5 Sets | ||
| Resistance band, while performing Soccer skills to mimick opposition off balancing | Perturbation: Side/fwd/back Mvt Passing Shooting | 1min x 5rep Each drill | ||
| Functional Specific Skill – Build confidence | Shooting Session with Goalkeeper | 15 mins | ||
| Sport Specific, agility, speed, accelearation, deceleration, passing | Jog Pass, Sprint, to cones in different directions | 15 mins | ||
| Warm down | Warm Down – slow cycle Passive stretch/Foam roller | 10 mins |
Return to Sport Assessment
Return to sport testing and assessment should be conducted through an objective analysis of lower limb strength, functional kinematics as well as ability to integrate to specific demands of the sport. Physiological (39) and psychological readiness also play a significant role. (32) Isokinetic strength of Quadriceps and hamstrings, as well as hop tests described in initial assessment should have >90% co-symmetry. (40) (41).
Tuck Jump and single leg squat assessments can be used to test asymmetries. (42)
For the Psychological component we can use the “12-Item ACL-Return to Sport (ACL-RSI) scale”. (39)
Sport Specific readiness assessed through systematic increases of load and subjective monitoring, of sport specific functions movement, and fitness levels.
___________________________________
Week 12 – If player has passed all tests – Resume training with Team – A multi-disciplinary approach with a Sports Psychologist for mental readiness of athlete in process would be ideal.Evidence based Approach of ACL Rehabilitation without surgery – Identification and progression of “Coper” with Conservative management
Author:
Constantinos Hadjichristofis – Bcom Human Resource Managment (Wits) PT (ACSM) BSc (Hons) Physiotherapy (Herts) MSc – Sports Medicine, Exercie and Health (UCL).
